For
The Love of Your Heart
Easy Esselstyn Diet Recipes
with Pictures: Stories
|
Stories |
|||
|
Klaus Daily Meal Pictures for over three Months Challenge Study Meals for two Months |
Why to change your American Red-Meat/Processed-Food Diet having
30%-Fat? Klaus’ Story: I thought that I was
living a healthy life style including modest eating habit, no smoking, little
social alcohol consumption and infrequent physically challenging activities
(bike riding and summer hiking). At work I had little stress and at home I
consumed the typical American Diet (30% fat) of almost daily red meat and
processed foods (like high sodium orange juice, chips, cheese, sour cream
etc.) and never really cared about my blood work done for my yearly
physicals. I felt great and healthy. Then I realized that I was slowly
gaining weight and changed my diet to what is called a Mediterranean Diet
(20% fat) of vegetables, salads, fruits and white meat (chicken and fish)
using olive oil for cooking. Reducing my cholesterol levels, as can be seen
in the chart of the table below, it did not affect the silently progressing
disease of my coronary heart vessel blockage leading towards inevitable heart
failure because my cholesterol never fell below the critical thresholds
essential for preventing heart failure (dashed lines in the chart below). Then,
one day while mowing the lawn I felt a strong diffuse chest pain and
consulted my Family Doctor. The Resting ECG (Electro Cardiogram) looked great
and normal. For evaluation of my complaints he sent me to a Cardiologist for
a stress test. I did not pass the test and on the spot was rushed with an
ambulance to the Emergency Room for Quadruple Bypass Heart Surgery:
I was with no minutes to spare very, very close to heart failure and permanent heart damage. Under exceptionally professional and loving care by nurses and doctors I left the hospital five days later. During my rehabilitation I learned too late all about the risk factors for heart disease but no concrete specific advice was given on healing my diseased heart except for some general guidelines on to moderate my (American Diet) eating habit, quite smoking (I do not smoke), exercise often (OK) and reduce stress (OK) and blood pressure (was and is OK). So I continued with my Mediterranean diet but added more gym time (2-3 times a week). Hearing from a friend and Googling Heart Disease I learned about and started to read doctors Ornish’s and Esselstyn’s books on how to “heal” my diseased heart. If I would not change my life style my newly implanted artery and veins that now supply my heart would clog with new cholesterol plaques and I would need another bypass operation in ~ 5-10 years. But this message really did not sink into my consciousness until by chance I saw a CNN-interview of former President Bill Clinton regarding the failure in 2010 of his 2004 quadruple bypass and his lifestyle change to Esselstyn’s diet. Esselstyn’s advice on healing a diseased heart is simple but dogmatic in that I would have to radically change my lifestyle and eating habits! The interview was encouraging me to do it and take the first steps. |
|
|
|
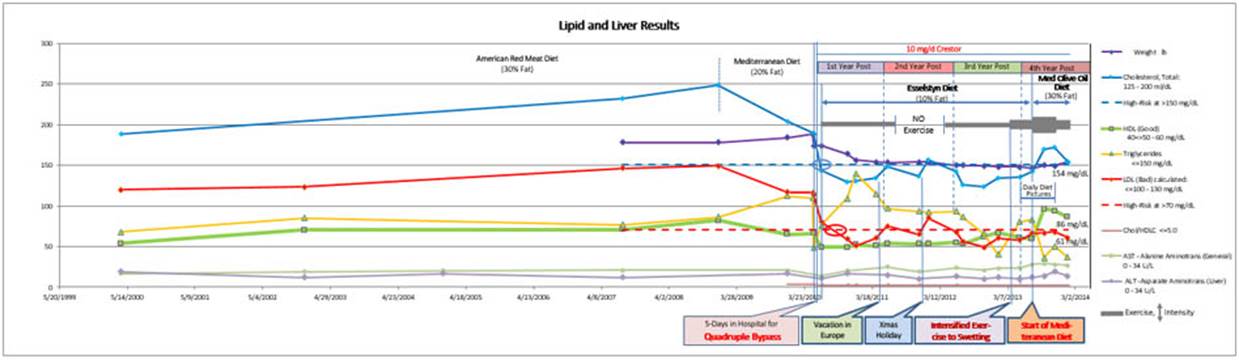
Table: 14 years of charted blood component concentrations and body weight.
The data points reflect the blood values at the end of the measuring interval
and may represent the influences of all variations in-between depending on their
persistence which is at this time widely unknown. (Chart detail for diet
years below). |
|||
|
|
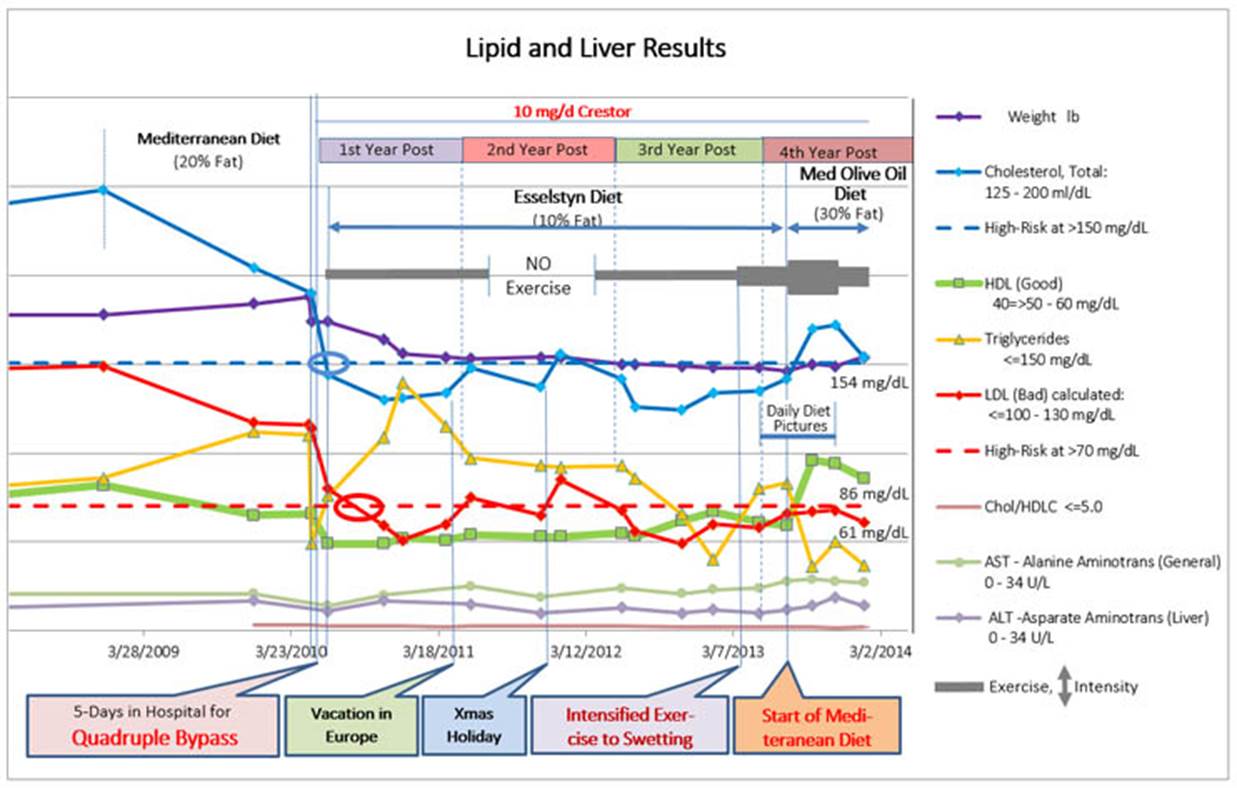
The diet experience. Starting the dieting
journey seemed daunting and surreal at first but I figured it out and adapted
to it. Now I am working out every day for 60 min at the local gym and
following strictly Esselstyn’s advice. It was a steep learning curve, cooking
for myself, finding and selecting the appropriate foods and grocery items and
managing my new lifestyle. Already after only four weeks being on the
Esselstyn-based diet my LDL (red: bad cholesterol) had dropped significantly
below the high-risk ceiling of 70 mg/dL and my total cholesterol (blue)
stayed almost always below the safe level of 150 mg/dL. At these conditions
coronary heart disease is not diagnosed. I am now feeling great knowing that
my heart is healing (probably reversing plaque growth and opening up clogged
vessels) and my newly implanted blood vessels will be staying healthy without
getting further diseased. However, this diet system includes many diverse
components and their relationships and effects on measured blood values is
not easily understandable and more or less hidden to both the patient and the
physician, because for most patients it is hard if not impossible to reliably
follow a physician’s even mostly general advice. Additionally, the individual
diet response may vary from patient to patient. As I found out in the second
diet year, short-term deviations from the diet would have dramatic
longer-term effect on the cholesterol levels. I am a scientist and set out
from the start of my dieting to take control of my own health destiny by
critically observing the effects of Esselstyn’s prescriptions on a daily
basis. These are my results and my generalized conclusions. The
chart covers in detail the first years after my heart operation and shows my
blood and weight values related to my diet and some special living events
that occurred since then. It is easily recognizable that there are two groups
of values each changing in their own but very different ways. The
triglycerides (yellow line), weight (purple line) and HDL (good cholesterol:
green line) indicate longer-term adaptation and specific interactions with
each other while the total cholesterol (blue line) as well as the LDL (bad
cholesterol: red line; calculated from the total cholesterol and the HDL)
indicate short-term adaptations to life style changes and parallel
interactions with each other. In
the first diet year I lost 30 pounds regaining my adolescent
school-sport-supported weight which I could maintain in the following years.
However, in the first half year, when my initial weight reduced rapidly, my
triglycerides (yellow) increased steeply, a relationship reported in the
medical literature to be closely related. The triglycerides fell back as
steeply and then stabilized to a plateau for nearly one year before dropping
off again as rapidly to their lowest value yet of 35 mg/dL and then increased
again while the weight reduced only minimally. In contrast, my HDL
(good/green) showed only small variations between 50-70 mg/DL. It was
initially steady over two years but thereafter started to increase at a
similar time the triglycerides where again dropping. Both desirable changes
cannot yet be correlated with other events but it may be that changes are
responding to those of eating habits when I was falling back to
conventionally sized portions (see below) and increasing physical activity
(thicker line indicating activity increase to sweating). The
total cholesterol (blue) and LDL (bad/red) cholesterol appear to react
rapidly and in tandem. Two increases in the second year after the operation
followed a vacation and a holiday season. On these two occasions I was
breaking the diet rules for only a few days. After the vacation incident
(consuming “irresistible” fatty and sugary pastries) elevated LDL (bad/red)
values reach 65mg/dL and after the holidays (consuming sugary foods and a lot
of wine) an even higher value of 85 mg/dL is observed. The rapid increase of
the cholesterol values and the slow recovery over months reveal a high sensitivity
of these two blood components to “breaking the diet rules” for only a few days
despite close adherence to the rules before and immediately afterwards. In
the third year I paid special attention not to break the rules and both values
although fluctuation stayed below the desirable maximum (dashed lines). Unfortunately,
due to a severe sciatic nerve irritation during the summer preceding the Xmas
holidays I had to stop my gym exercises for 7 month but could pick them up
again after the holidays. This lack of exercise might have been the reason
that excess calories were not burned away fast enough causing an accentuated
increase of LDL (bad/red). Cholesterol increase from excessive calories is
well documented. It underscores that low calorie consumption as well as
exercise are an import part of this diet. As a precaution against further
unintended minor missteps I changed to a very low fat diet, reducing fat
intake wherever possible, especially for breakfast (lowest-fat granola and
non-fat soy milk), lunch (low-fat pita flat breads with no-fat hummus) and
dinner (using if called for only low-fat tofu products). My new lifestyle. It took me three years to get a grip of my
new way of living. In the first year my body was physiologically adjusting.
During the second year I was learning psychologically to live with it. And
only in the third year I was gaining a deeper understanding of the mechanisms
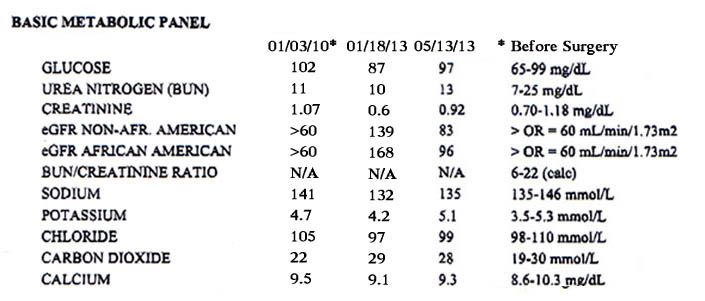
and their control. Meanwhile, my basic metabolism remained quite healthy when
comparing the pre-operative and post-operative values. The recent values (see
table below) were measured in the same blood sample as used at the end of the
third year (analyzed to monitor my kidney function under treatment with the
diuretic Furosemide).
The
undesirable sodium and chloride are at the minimum, and desirable potassium
and calcium are in the mid-range. The glucose is close to the maximum but
Furosemide might have affected this value. However, I should watch my
sugar/calorie intake. It may also help to lose some few extra pounds since I
am definitely not skinny. My
lifestyle now includes besides of a very-low fat diet, low sodium as well as
daily exercises (burning around 400 calories) also low-sugar intake in
support of controlling my calorie balance. These changes will help
maintaining my “exceptional good” blood values as my cardiologist just told
me after seeing my latest now stabilized blood analysis results after the third
year post operation. Living on a controlled diet needs attention to EVERY
detail WITHOUT exceptions, as Esselstyn repeatedly stresses in his book and I
am starting to realize now. In
addition to everything known for maintaining good heart health (Gillinow and
Nissen: Heart 411) Dr. Caldwell Esselstyn’s advice for healing a diseased
heart is a “10% Fat and Plant-based Diet” without any cholesterol intake from
animal products, low-salt content, no plant oils and includes the reduction
of the natural liver production of cholesterol by daily exercise and low
dosage (10mg) of a statin (Crestor). Optimal blood values are for Total
Cholesterol below 150 mg/dL and LDL (bad cholesterol) below 85 mg/dL. At risk
patients with heart disease should have a LDL (bad cholesterol) level below
70 mg/dL (see chart dashed lines). These are now widely accepted threshold
values.
In general, a 10% fat diet requires detailed consideration of the nutritional intake in regards to low-fat, low-salt and low sugar content. In the ‘Finding Products’ charts I label those items with a special conformance icon for easier recognition. Please contemplate that plants used for dinner preparation already provide approximately one half of the daily allowance for fat (5%) meaning that only 5% fat is available for the remaining ingredients used for the preparation of dinner, breakfast, lunch and snacks. This is only possible by using ingredients that are for practical reasons fat-free and have per serving a fat content of only 1% or less of the Daily Value as prescribed in the dietary guidance of the Food a Drug Administration (FDA). Such a practice is very cumbersome to follow since it requires constant consultation of food labels. Gone are for breakfast stone rolled oatmeal (1/2 cup has a 5% daily value of fat) and light almond milk (1/2 cup has an additional 2% fat). Inclusion of flax seed flour for supplementing the Omega 3 intake will already introduce 4.6 % fat. And having some bread with hummus for lunch is challenging as well. One slice of salt-free whole grain bread may have 1-1.5% of fat and the choice for fat-free hummus without tahini is limited. There are low-fat or fat-free products available in health food stores and increasingly in supermarkets but it is tedious to find them and remember where they are sold and in which isles they are placed. Well, this is the flip side of staying healthy when having highest risk factors for heart disease. Lucky are those who do not (yet) fall into this category. Weight and Calories. I found
daily weight control very helpful if performed at similar physiological
patterns, i.e., in the morning after bowl movement (being like clockwork in
plant dieting), exercise and shower. If the weight is found to be too high
over several days than it is easy to reduce the calorie effects by exercising
more or eating less (my favorite meal for that purpose is the Yellow Turnip
Vegetable Soup – 005 or some of the Quick Meals. Also drinking plain iced
water instead of juice or wine helps.) In the first two year of 10%-fat-plant
dieting I had a nearly unsatisfyable appetite eating more or less two
portions for one meal and was feeling afterwards heavy and tired while retaining
approximately 4-5 pounds in weight. Now, I am down to more regular portion
sizes and feel much better having also lost the initially remaining extra
weight although I am still have some pounds to go. This energy balance is
essential for maintaining a normal physiology because depleting calorie
intake too much changes the physiology from healthy calorie burning activity
mode to unhealthy starving mode where non-essential calories are converted to
liver fat increasing triglyceride and cholesterol levels. The Daily Practice. Esselstyn-based
dieting necessitates framing your personal life with a regular schedule of
exercise, cooking and shopping but also provides inner instinctive
satisfaction from the enjoyment of preparing the meals, working with natural
ingredients and tasting natural flavors. This site will start you in the
right direction for the latter two activities cooking and shopping. The rest
is up to you. The Challenge of Gillinow and Nissen: FOOD FIGHTS Draft - Klaus Peters*) We
need more detail studies on the relationship between lifestyles and hear
health. Two widely publicized very-low-fat diets for maintaining heart-health
(Ornish, 2007; Esselstyn, 2007), were recently challenged by a third high-fat
approach based on olive oil (Gillinow and Nissen, 2012). It took me over
three years post operation to grasp the impact of my diet choices on my
cholesterol levels and I felt ready to test the proposed high-fat approach in
a challenge study. After staying for more than one year (see data in chart: 3rd
Year Post) on Esselstyn’s diet below high-risk levels for cholesterols, I did
not change anything in my lifestyle except including the recommendations of
Gillinow and Nissen. Both diets embrace low-dose statin application, in
contrast to the Ornish diet that rejects it. For this comparative study I
documented with pictures my daily meals and lifestyle for two months before (see
Daily Meal
Pictures for over three Months) the diet
change and four month afterwards (Challenge
Study Meals for four Months). The
results of the very-low fat diet showed that I could control my dietary
intake exactly as prescribed by Esselstyn with the result of my total
cholesterol staying below the recommended level of 150 mg/dL, and of LDL
below the high-risk threshold of 75 mg/dL. With this baseline being
established for over one year moved to and stayed on the
Gillinow-Nissen olive-oil-based Mediterranean Diet (2.5 tablespoons of extra virgin
olive oil per day) maintaining everything else in my lifestyle. So in fact,
only my meal composition changed from 10% to ~30% of
Recommended-Daily-Allowance Calories coming from “good” fats, which derive
from plants and now as well as from olive oil, nuts, chocolate, chicken and
fatty fish. The abrupt diet
change did not caused any digestive problems. The recommended olive oil and nuts added some 500 calories per day, which required me to double my daily exercise in the gym to two hours per day combined with heavy sweating in order to maintain my weight at 148-150 lb. However, after four month I had to scale back the workout by 40% and accept a 6 pound weight increase. But what did the olive oil and the fish fat do? It is clear that the HDL increased sharply. Surprisingly, the LDL did not change and stayed below the at risk levels contrary to the total cholesterol that increased in tandem with the HDL. In addition, the Triglycerides deceased to lowest levels. So, effectively the olive oil (in combination with increased of physical activity) decoupled the LDL and the total cholesterol, which were under very-low fat-diet changing in tandem. This puts a new light on the LDL values since they were little affected by the HDL. The increase of the total cholesterol above the “at risk” level is due to the HDL. Changes in weight and small fluctuations in triglycerides levels may mirror the problem of weight control in this high-caloric diet. |
|
|
|
Figure 1: Blood
values and weight of a single patient who is a male Caucasian of 73 years in age
(at data end points); Blood pressure 60/120 , weight 156 lb, height 6’ 1’’; Non-smoker;
Only low social alcohol consumption; No other major health problems. Chart
Detail: After 10 years of steadily concomitant increase of all values (not
shown in figure) the cholesterol values could be decreased by diet
modification to a conventional Mediterranean Diet (20% fat) combined with
occasional physical activities. However, this could not stop the progressing
cardiac disease leading to an emergency quadruple bypass operation. During
the following 3 years while a very-low fat diet was followed, the first year
showed a dramatic weight reduction and concomitant triglyceride peak, the
second year reflected short-term diet deviations, and the third year
demonstrates expected outcomes below risk-thresholds at full diet compliance.
The last six months reflect the outcome and maintenance of blood component
values while following an olive-oil & nuts Mediterranean diet. |
|||
|
|
Both diets (Esselstyn’s very-low fat vegan diet and
Gillinow-Nissen’s high-fat Mediterranean diet) are based on scientific
hall-mark large-scale studies (Chinese Study, Mediterranean Study) and can be
fully verified when compared side-by-side under self-guided physiological
conditions in a controlled single person study under low-dose statin
conditions. Both diets can maintain LDL levels below 70 mg/dL. The
Mediterranean olive oil-based diet provided the additional benefit of almost
doubling HDL levels but at the cost of unrealistically demanding exercise
levels (2 hrs sweating per day) for weight preservation. On the other side,
the very-low fat diet (Esselstyn 10% fat diet) is also demanding because it
does not allow any even minor deviation (from consumption of “bad” fats and
excessive calories from alcohol and sugars) without severe long-lasting
consequences of elevated LDL levels (see second year post OP). Conclusions: On the background of the recently
recommended increase of the statin usage for cholesterol maintenance (CDC,
2013), the Esselstyn diet and the Gillinow -Nissen diet strategies should
be fused so as to ease weight control. A reduction of olive oil and fish oil
consumption and an increased inclusion of very-low fat plant meals provide a
promising flexible diet avenue while maintaining all the other established
essential lifestyle practices common to both approaches, like whole-grain
flour products, “good” carbohydrates, fruits, nuts, dark chocolate, red wine
as well as daily extensive exercise combined with no smoking, normal heart
rate, low blood sugar levels and normal body weight. In practice, this is
what the Ornish diet prescribes, but including olive oil and replacing
the requirement of meditation, group therapy and yoga (for stress reduction)
with a low-dosage statin application. So, in the end, all three diet
approaches, heavily publicized through books, media appearances and some
polemic commenting, should be fused for providing a realistic practical
approach to good cardio-healthy lifestyle: It’s not exclusively either
very-low fat dieting, statin barring at all cost, or unlimited olive-oil
consumption, but a measured approach using all three aspects tailored to the
physiological and pathological situation of the individual patient. There is
and will be always more that we should know about heart health and it is the
scientific comparative approach that will make us understand better the
complex human system and guide us in improving health, happiness and
longevity. References Esselstyn CB, Prevent and Reverse Heart
Disease. Avery, NY, 2007. Ornish
D. Dr. The Spectrum: A Scientifically Proven Program to
Feel Better, Live Longer, Lose Weight, and Gain Health. Ballantine
Books, New York NY, 2007. Gillinov
M and Nissen S. Heart 411: the only guide to heart health you’ll ever
need. Three Rivers Press, New York NY, 2012. Estruch R, Ros E,
Salas-Salvadó J, Covas MI, D
Pharm, Corella D, Arós F, Gómez-Gracia E,
Ruiz-Gutiérrez
V, Fiol M, Lapetra J,Lamuela-Raventos RM,
Serra-Majem L, Pintó X, Basora J, Muñoz
MA, Sorlí JV, Martínez JA, Martínez-González MA; the
PREDIMED Study Investigators. Primary Prevention of Cardiovascular
Disease with a Mediterranean Diet. N Engl J
Med. 2013 Feb 25.
[Chinese Study]
[Mediterranean Study]
[CDC Recommendations, 2013]
*) Dr. Klaus Peters is a biologist and computer
scientist at the Southern Connecticut State University, Computer Science. |
|
|
|
Bill Clinton’s Story at http://www.vegsource.com/news/2010/09/cnn-interviews-caldwell-esselstyn-md-dean-ornish-md-about-bill-clintons-plant-based-diet.html (excerpts below from that website) Caldwell Esselstyn Jr.
MD & Dean Ornish MD Explain Bill Clinton's Diet To CNN CNN.COM | 09/24/10 On Friday, September 24,
2012 CNN's Wolf Blitzer interviewed Caldwell Esselstyn Jr MD and Dean Ornish
MD, the doctors whose diet former President Bill Clinton has used to
successfully return to his high school weight -- and to reverse his serious
heart disease. Background: In 2004 Clinton underwent quadruple bypass
surgery, taking four veins from elsewhere in his body and using them to
circumvent the four blocked arteries to his heart. In 2005, Clinton
underwent more surgery, for scar tissue damage and fluid which had
accumulated as a result of the 2004 surgery. In
February of 2010, Clinton's bypass failed, with one of the four veins
installed in the bypass having become 100% blocked. Surgeons installed two
stents inside the clogged vein, in order to prop open the cholesterol-filled
passage. In May
of this year, Clinton began Dr. Esselstyn's plant-based diet program, which has been
shown in published research to arrest and reverse heart disease in 100% of
people who are compliant with the diet. Over the next few months,
Clinton lost 24 pounds, returning to his high school weight, feels great, and
his heart disease is in reversal. Video: The CNN video below starts with about a
minute of Clinton's interview, then cuts to several minutes of riveting
commentary from the two esteemed plant-based doctors responsible for this
health-turnaround. Click picture to watch YouTube video. |
|||
|
|
|||
|
|
|
||
|
Comments: Write to heart@youworldtree.com and we
will add your contribution here. |
|||